For millions of hopeful parents around the world, in vitro fertilization (IVF) is a journey filled with faith, science, and resilience. IVF offers couples dealing with infertility the opportunity to conceive through assisted reproductive technology (ART). However, despite its impressive success rates, it is not foolproof.

Globally, IVF outcomes vary — research by the ASRM shows that women below 35 typically record a 35–40% success rate per treatment, while those approaching 40 often experience a 20%–25% rate. This decline reflects the natural reduction in ovarian reserve and egg vitality with age, according to the American Society for Reproductive Medicine (ASRM).
When a cycle does not succeed, the disappointment can be intense, often leading to feelings of grief, confusion, and self-blame. However, it is important for every patient to understand: IVF failure does not equate to personal failure. It is a medical occurrence affected by various biological, genetic, and lifestyle factors – many of which can be managed with appropriate diagnosis and treatment planning.
The Importance of Egg Quality and Maternal Age
The single most decisive factor for IVF success is the biological quality of a woman’s eggs which is a reflection of both age and underlying health conditions. By the time a woman reaches 40, over 60% of her eggs may have chromosomal issues, which can cause failed implantation or miscarriage.
If you are over 35, your doctor might recommend:
- Freezing eggs at a younger age for later use.
- Using donor eggs, which typically have higher success rates (50–60% per cycle).
- Preimplantation Genetic Testing (PGT-A) to check embryos for chromosomal issues before transfer.
While these methods do not completely remove risks, they significantly enhance your chances of success in future cycles.
Factors Affecting Male Fertility
About 40–50% of infertility cases involve male factors. Low sperm count, poor movement, and abnormal shape can hinder fertilization and embryo quality. Even minor DNA damage in sperm, known as sperm DNA fragmentation, can cause early embryo failure.
Modern methods like Intracytoplasmic Sperm Injection (ICSI) and sperm DNA fragmentation testing can help identify and resolve these problems.
Making lifestyle changes – such as quitting smoking, reducing alcohol intake, improving sleep, and maintaining a healthy weight – can enhance sperm quality within three months, which is the typical sperm maturation period.
Embryo Viability and Genetic Health
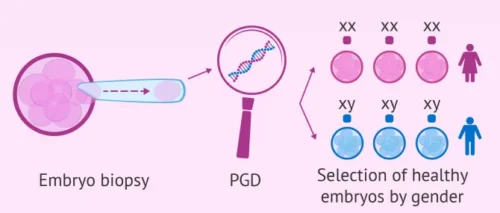
Not all embryos are viable, even if fertilization is successful. Clinical studies in reproductive genetics reveal that roughly half of all IVF-generated embryos carry chromosomal errors, explaining many implantation or early miscarriage cases.
Advanced screening technologies like PGT-A and time-lapse imaging enable embryologists to choose embryos with the best chances of development. This approach to precision medicine boosts success rates and lowers the likelihood of multiple failed cycles.
Uterine Receptivity and Structural Challenges
A healthy embryo requires a receptive uterus for implantation. Hidden reproductive disorders – such as undiagnosed endometriosis, uterine fibroids, or adenomyosis – can subtly distort the uterine environment, blocking successful embryo attachment.
Moreover, a thin endometrial lining (under 7mm) can greatly decrease the chances of implantation. Diagnostic tests such as:
- Hysteroscopy,
- Saline infusion sonography, and
- Endometrial receptivity analysis (ERA) can reveal hidden uterine issues.
Treatment options may include minor surgery, hormonal therapy (support with oestrogen or progesterone), or platelet-rich plasma (PRP) therapy to enhance endometrial health.
Hormonal Balance and Ovarian Response

The effectiveness of IVF relies on a precise hormonal sequence – particularly FSH, LH, oestrogen, and progesterone. If your body does not respond consistently to stimulation drugs or if luteal phase hormones are insufficient, implantation could fail.
Conditions such as polycystic ovary syndrome (PCOS) or thyroid issues can affect hormone levels. Modifying medication dosages, using gentler stimulation protocols, or providing luteal support can help balance hormone responses and boost success rates.
READ ALSO: 7 Daily Habits That Can Cause Br3ast Sagging and How to Avoid Them
Immunological and Genetic Factors
Sometimes, the immune system may wrongly see an embryo as a foreign body. Immunological rejection, high levels of natural killer (NK) cells, or autoimmune disorders can interfere with implantation.
Although debated, some fertility experts use immune-modulating treatments, like corticosteroids or intralipid infusions, when tests indicate immune involvement.
Couples experiencing repeated IVF failures may also have balanced translocations or other chromosomal variations. Genetic counseling and PGT-M (Preimplantation Genetic Testing for Monogenic Disorders) can effectively identify and manage these risks.
Lifestyle and Environmental Influences
Scientific research consistently indicates that factors like nutrition, exercise, stress, and exposure to toxins affect fertility outcomes. Factors that are known to lower IVF success include:
- Smoking cigarettes – decreases ovarian reserve and sperm quality.
- High alcohol and caffeine consumption – associated with reduced implantation rates.
- Obesity or significant weight loss – disrupts hormonal balance.
- Contact with environmental toxins such as BPA (found in plastics) and pesticides.
Eating a Mediterranean-style diet, which is high in antioxidants and omega-3 fatty acids, can improve the quality of eggs and sperm. Engaging in regular moderate exercise and practicing mindfulness to reduce stress also promote reproductive health.
The Emotional Burden

Emotionally, IVF can be one of the most draining medical journeys a couple faces – each cycle blending hope, fear, and exhaustion. Ongoing stress raises cortisol levels, which can indirectly impact reproductive hormones like LH and FSH.
Counseling, fertility coaching, and mind-body programs (such as yoga, meditation, and guided therapy) have been shown to enhance emotional health and even improve IVF results. Some couples find solace in peer support groups, where shared experiences help restore hope and perspective.
Learning From Each Cycle
A failed IVF cycle provides crucial clinical information. Analyzing details such as fertilization rates, embryo quality, uterine thickness, and hormone levels helps doctors improve their methods. Often, modifying medication dosages, altering the timing of embryo transfers, or changing laboratory techniques can lead to better outcomes.
Consider each cycle as a learning opportunity rather than a setback. IVF is becoming more personalized, and ongoing learning from your experiences is an essential part of the process.
KEEP IN MIND: Medical advancements in assisted reproduction continue to evolve, offering new possibilities for couples.
Author: Dr. Abayomi Ajayi, MD, FRCOG (UK)
Dr. Abayomi Ajayi is a consultant obstetrician and gynecologist with over 25 years of experience in reproductive medicine and fertility management. He is the founder of Nordica Fertility Centre, Lagos, and a fellow of the Royal College of Obstetricians and Gynaecologists (UK).


[…] IVF Failure: Causes, Emotions and How You Can Improve Next Cycle […]